Medical Billing
Information for each patient encounter is used for medical billing. The DX (condition of the patient) and CPT (service rendered to the patient) are used when generating proper medical codes for billing. ICD-10 and CPT codes can easily be extracted from the patient encounter and entered into an invoice used for medical billing. The coding information is used to generate HCFA 1500 (CMS 1500) forms for insurance submission or the information can be submitted electronically through EDI (Electronic Data Interchange) to a medical billing clearinghouse. WebShuttle will guide you through the medical billing process with tools and reminders that make it easy.
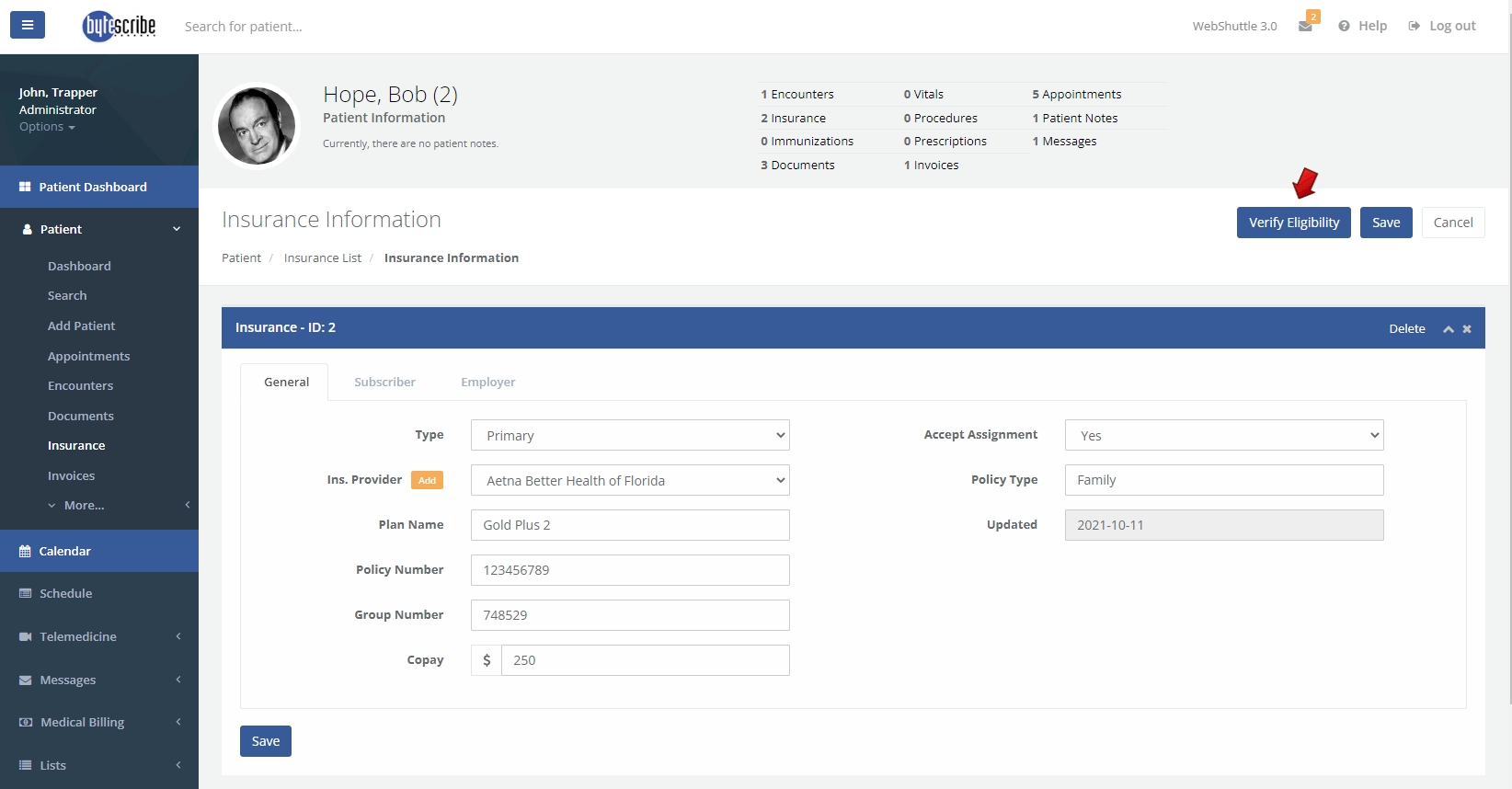
Insurance Verification
It is necessary to verify patient insurance information to ensure that eligibility and policy benefits are documented. This determines whether the insurance claim can be obtained for services rendered. Patient responsibilities such as co-pay, deductibles and out-of-pocket expenses need to be entered. With some services, prior authorization is required from the insurance company.
Patient Encounters
When the provider encounters a patient during an office visit or telemedicine call, the details of the condition and service are documented in the EHR system. Audio or video are sent for transcription and all results are documented. The details can be recorded during the encounter or after the visit or call. Information about the medications and condition are all documented. Information from the encounter is used during coding.
Transcription
Recorded audio or video is routed for medical transcription. The transcriptionist will convert audio to standard documents such as a History and Physical, Consultation, Operative Report, Letter, Discharge Summary or any custom document. Transcribed documents are automatically attached to the patient chart in the EHR system. The transcribed document contains the complete condition of the health record. Information from medical transcription will be used during coding.
Medical Coding
Medical codes are extracted from the transcribed information. The patient's condition, medical services rendered, medical prescriptions are all converted into medical codes. The complete medical history is condensed into medical codes. Experienced medical coders are often involved in the medical coding process. Coders usually extract the DX (condition of the patient), CPT (service rendered to the patient) when generating proper medical codes for billing.
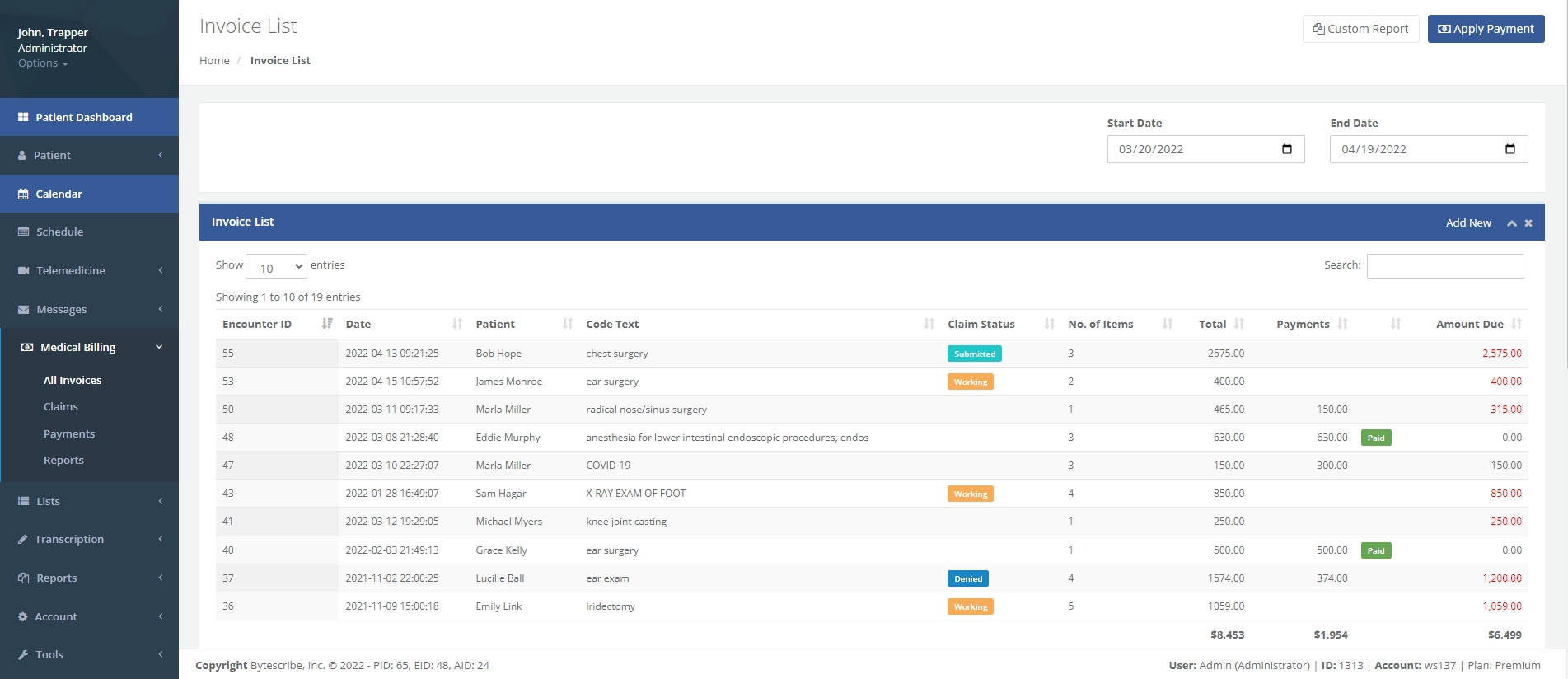
Entering Medical Charges
Charges for services rendered will be entered into the patient invoice. Appropriate values are assigned to each of the services rendered. These charges will then be sent to the medical billing company (clearinghouse) or directly to the insurance company for a claim. The billing sheet must be complete and free of errors or it may reflect during a claim. Accuracy is very important during claim submission.
Charge Transmission
Transmitting the claims to the insurance company is called Charge transmission. Electronic submission is called EDI (Electronic Data Interchange). EDI is secure and encrypted. Claims need to be without errors when transmitting through EDI. Errors can result in the following:
1. Mandatory fields need to be filled without errors. Claims with errors will be rejected. 2. Invalid information in the patients health record will cause the claim to be rejected by the EDI. 3. Claims can be rejected due to insurance guidelines and payer details.
Denials need to be processed if a claim is rejected or not approved.
Calling about Denials
In many cases, it is necessary to to follow-up on denied claims to correct issues that prevented payment. Following up in a timely manner increases the chances of claims being paid. The goal is to receive payment for all services rending by the healthcare providers. Often, patient information is supplied and errors are rectified.
Denial Management
Learning from prior denials and taking appropriate actions to correct issues is an important step in improving RCM (Revenue Cycle Management). Denial management is an important step in maximizing payment for services rendered. Determining the causes of denials will reduce the risk of future denials. A proper course of action should be takes after evaluating denied claims by the denial management team. Denied claims should be prioritized by payers and amounts to maximize reimbursements.
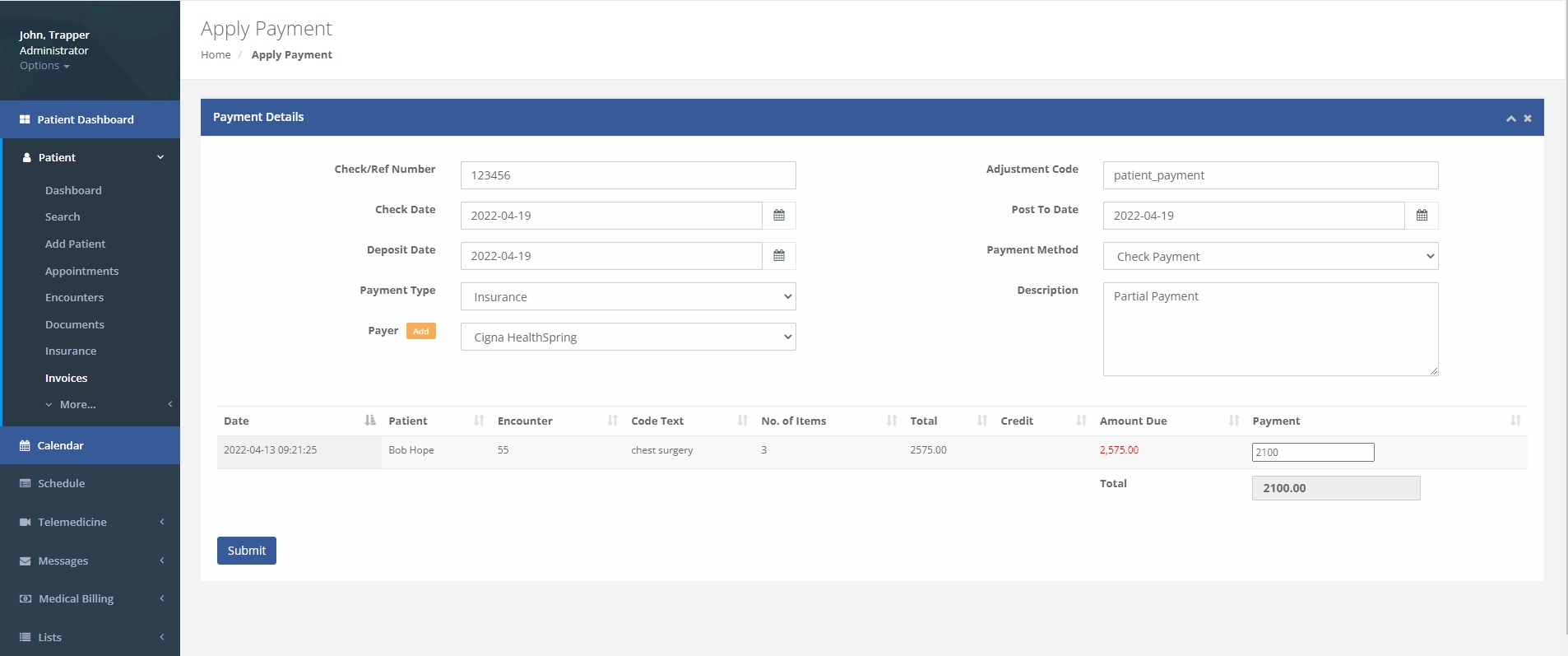
Posting Payments
Payments received will need to be posted into the EHR software. Correspondence, EOB (Explanation of benefits), and ERA (Electronic Remittance Advice) will received from the insurance companies. The proper amount will need to be posted to each invoice from bulk payment receivables.