Medical Billing
Information for each patient encounter is used for medical billing. The DX (condition of the patient) and CPT (service rendered to the patient) are used when generating proper medical codes for billing. ICD-10 and CPT codes can easily be extracted from the patient encounter and entered into an invoice used for medical billing. The coding information is used to generate HCFA 1500 (CMS 1500) forms for insurance submission or the information can be submitted electronically through EDI (Electronic Data Interchange) to a medical billing clearinghouse. WebShuttle will guide you through the medical billing process with tools and reminders that make it easy.
Medical billing is a crucial process in healthcare, ensuring that healthcare providers are reimbursed for their services. The following guide outlines the key steps involved in medical billing, from patient encounters to insurance verification and claims submission.
Patient Encounters
During a patient encounter, whether it's an office visit or a telemedicine call, the provider documents the details of the patient's condition and the services rendered in the EHR (Electronic Health Record) system. This includes:
- Recording Condition and Services: Detailed documentation of the patient's condition and services provided.
- Transcription: Audio or video from the encounter is sent for transcription. Transcriptionists convert this into standard documents (e.g., History and Physical, Consultation, Operative Report).
- Documentation: Transcribed documents are attached to the patient chart in the EHR system, capturing the complete condition of the health record.
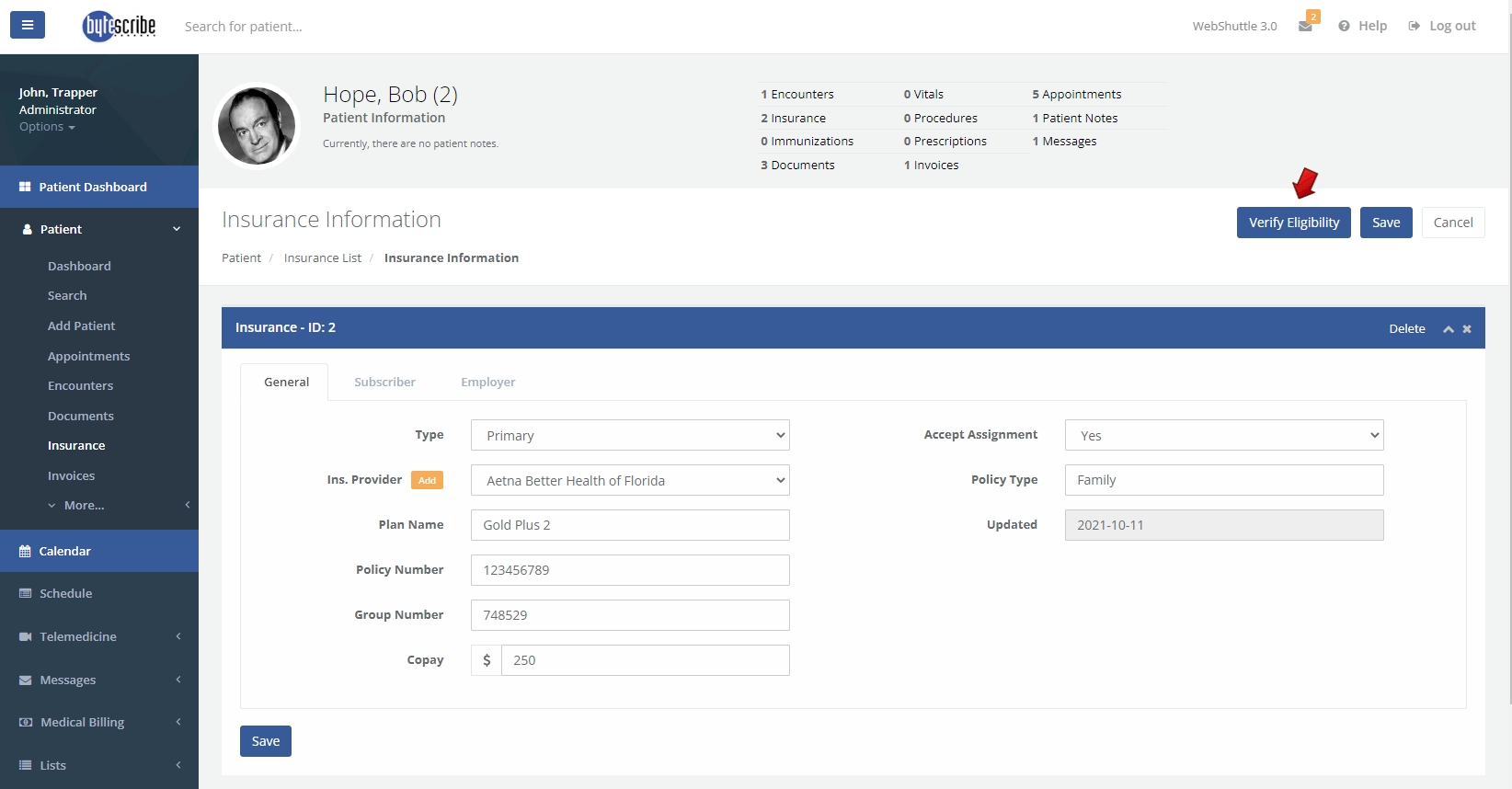
Insurance Verification
Verifying patient insurance information is essential to ensure eligibility and policy benefits are documented. This step includes:
- Eligibility Check: Confirming that the patient’s insurance is valid and active.
- Policy Benefits: Understanding the coverage details, co-pays, deductibles, and out-of-pocket expenses.
- Prior Authorization: Obtaining necessary authorizations from the insurance company for certain procedures or treatments.
<img src="path/to/your/insurance_verification_image.png" alt="Insurance Verification">
Medical Coding
Medical coding involves extracting codes from transcribed information to represent the patient's condition and services rendered. This process includes:
- ICD-10 and CPT Codes: Using standardized codes to describe the patient's condition (DX) and services rendered (CPT).
- Coder Expertise: Experienced medical coders review and assign appropriate codes to ensure accuracy.
Entering Medical Charges
Charges for services rendered are entered into the patient invoice. This involves:
- Assigning Values: Each service is assigned a specific charge based on standardized rates.
- Invoice Creation: The billing sheet is prepared, ensuring it is complete and error-free.
Charge Transmission
Submitting claims to the insurance company is a critical step, known as charge transmission. This can be done electronically through EDI (Electronic Data Interchange). Key points include:
- EDI Submission: Secure and encrypted electronic submission of claims.
- Error Checking: Ensuring all mandatory fields are correctly filled to prevent claim rejections.
<img src="path/to/your/charge_transmission_image.png" alt="Charge Transmission">
Denial Management
Handling denied claims involves:
- Follow-Up: Timely follow-up on denied claims to correct issues and increase the chances of payment.
- Evaluation: Understanding the reasons for denials and taking corrective actions to prevent future issues.
- Prioritization: Focusing on high-priority denials by payer and amount to maximize reimbursements.
Posting Payments
Once payments are received, they need to be posted in the EHR system. This includes:
- EOB and ERA: Processing Explanation of Benefits and Electronic Remittance Advice from insurance companies.
- Payment Posting: Applying the correct payment amounts to each invoice from bulk payments.
Example Screenshots
Invoice List
<img src="path/to/your/invoice_list_image.png" alt="Invoice List">
The invoice list shows detailed information about each patient encounter, including encounter ID, date, patient name, code text, claim status, number of items, total charges, payments, and amount due.
Apply Payment
<img src="path/to/your/apply_payment_image.png" alt="Apply Payment">
The apply payment screen allows administrators to enter payment details, including check/ref number, check date, deposit date, payment type, payer, and payment amount.
By following these steps, the medical billing process can be streamlined and efficient, ensuring accurate and timely reimbursements for healthcare services provided.
</body> </html>
Information for each patient encounter is used for medical billing. The DX (condition of the patient) and CPT (service rendered to the patient) are used when generating proper medical codes for billing. ICD-10 and CPT codes can easily be extracted from the patient encounter and entered into an invoice used for medical billing. The coding information is used to generate HCFA 1500 (CMS 1500) forms for insurance submission or the information can be submitted electronically through EDI (Electronic Data Interchange) to a medical billing clearinghouse. WebShuttle will guide you through the medical billing process with tools and reminders that make it easy.
Insurance Verification
It is necessary to verify patient insurance information to ensure that eligibility and policy benefits are documented. This determines whether the insurance claim can be obtained for services rendered. Patient responsibilities such as co-pay, deductibles and out-of-pocket expenses need to be entered. With some services, prior authorization is required from the insurance company.
Patient Encounters
When the provider encounters a patient during an office visit or telemedicine call, the details of the condition and service are documented in the EHR system. Audio or video are sent for transcription and all results are documented. The details can be recorded during the encounter or after the visit or call. Information about the medications and condition are all documented. Information from the encounter is used during coding.
Transcription
Recorded audio or video is routed for medical transcription. The transcriptionist will convert audio to standard documents such as a History and Physical, Consultation, Operative Report, Letter, Discharge Summary or any custom document. Transcribed documents are automatically attached to the patient chart in the EHR system. The transcribed document contains the complete condition of the health record. Information from medical transcription will be used during coding.
Medical Coding
Medical codes are extracted from the transcribed information. The patient's condition, medical services rendered, medical prescriptions are all converted into medical codes. The complete medical history is condensed into medical codes. Experienced medical coders are often involved in the medical coding process. Coders usually extract the DX (condition of the patient), CPT (service rendered to the patient) when generating proper medical codes for billing.
Entering Medical Charges
Charges for services rendered will be entered into the patient invoice. Appropriate values are assigned to each of the services rendered. These charges will then be sent to the medical billing company (clearinghouse) or directly to the insurance company for a claim. The billing sheet must be complete and free of errors or it may reflect during a claim. Accuracy is very important during claim submission.
Charge Transmission
Transmitting the claims to the insurance company is called Charge transmission. Electronic submission is called EDI (Electronic Data Interchange). EDI is secure and encrypted. Claims need to be without errors when transmitting through EDI. Errors can result in the following:
1. Mandatory fields need to be filled without errors. Claims with errors will be rejected. 2. Invalid information in the patients health record will cause the claim to be rejected by the EDI. 3. Claims can be rejected due to insurance guidelines and payer details.
Denials need to be processed if a claim is rejected or not approved.
Calling about Denials
In many cases, it is necessary to to follow-up on denied claims to correct issues that prevented payment. Following up in a timely manner increases the chances of claims being paid. The goal is to receive payment for all services rending by the healthcare providers. Often, patient information is supplied and errors are rectified.
Denial Management
Learning from prior denials and taking appropriate actions to correct issues is an important step in improving RCM (Revenue Cycle Management). Denial management is an important step in maximizing payment for services rendered. Determining the causes of denials will reduce the risk of future denials. A proper course of action should be takes after evaluating denied claims by the denial management team. Denied claims should be prioritized by payers and amounts to maximize reimbursements.
Posting Payments
Payments received will need to be posted into the EHR software. Correspondence, EOB (Explanation of benefits), and ERA (Electronic Remittance Advice) will received from the insurance companies. The proper amount will need to be posted to each invoice from bulk payment receivables.