Medical Billing
Medical Billing Overview
Medical billing is a critical part of the healthcare workflow, ensuring providers receive accurate and timely reimbursement for services rendered. VEHRDICT, in conjunction with WebShuttle, offers an integrated billing workflow that begins at the point of patient care and ends with payment posting.
From insurance verification to charge transmission and denial management, this guide outlines the full medical billing lifecycle.
---
Patient Encounters
All billing begins with a documented patient encounter—either in-person or via telemedicine. Providers are responsible for recording:
- Patient Condition (DX) and Services (CPT)
- Transcription of Encounter Audio/Video
- Final Documentation in EHR
Once transcribed, documents like H&P reports, consults, and operative notes are uploaded to the patient chart, forming the foundation for accurate billing and coding.
---
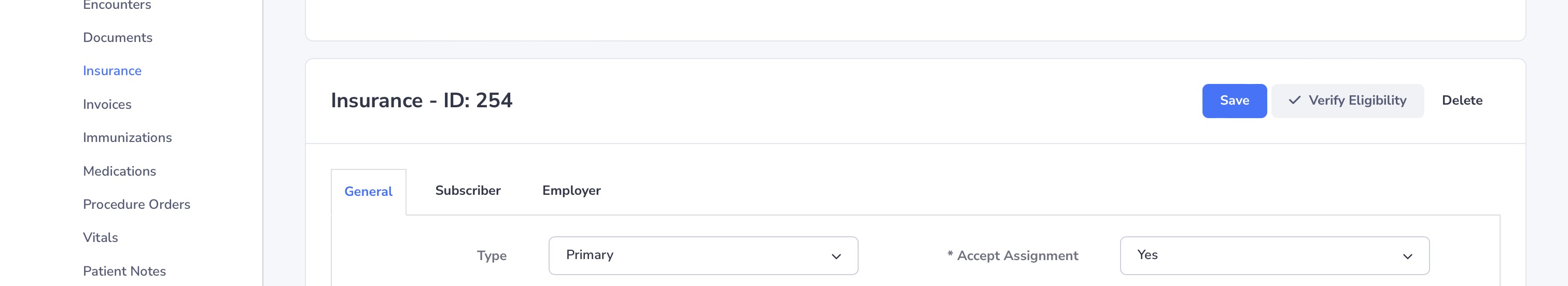
Insurance Verification
Before billing, it is essential to confirm the patient’s insurance status and understand their benefits. This ensures coverage and reduces claim denials.
- Eligibility Check – Confirm policy is active
- Policy Benefits – Review co-pays, deductibles, and coverage limits
- Prior Authorization – Secure approvals for procedures if required
---
Medical Coding
Once documentation is complete, coders extract:
- ICD-10 Codes – Patient diagnoses (DX)
- CPT Codes – Services performed
Accurate coding is vital for correct billing and compliance with insurance regulations. Experienced coders ensure codes reflect the medical necessity and scope of service.
Tip: Coding errors are one of the top reasons for claim denials. Always double-check code pairings and modifier usage.
---
Entering Medical Charges
Charges are entered into the system based on documented services:
- Assigning Charges – Each CPT code is linked to a standardized billing rate
- Invoice Creation – Review for completeness and accuracy before submission
This creates a billing record used for claim generation and submission.
---
Charge Transmission
Sending claims to payers is done via secure EDI (Electronic Data Interchange):
- EDI Submission – HIPAA-compliant, encrypted claim transmission
- Error Checking – Automated checks to reduce rejections
VEHRDICT tools assist in preparing, reviewing, and transmitting claims efficiently.
Tip: Use the EDI error checker to catch missing diagnosis codes, date mismatches, or NPI errors before submission.
---
Denial Management
For denied claims, follow-up is essential:
- Tracking and Follow-Up – Monitor status and resolve issues
- Root Cause Evaluation – Identify and address denial reasons
- Priority Handling – Focus efforts based on claim value and payer
Warning: Denials left unresolved can result in significant revenue loss. Implement a daily check of pending/denied claims.
---
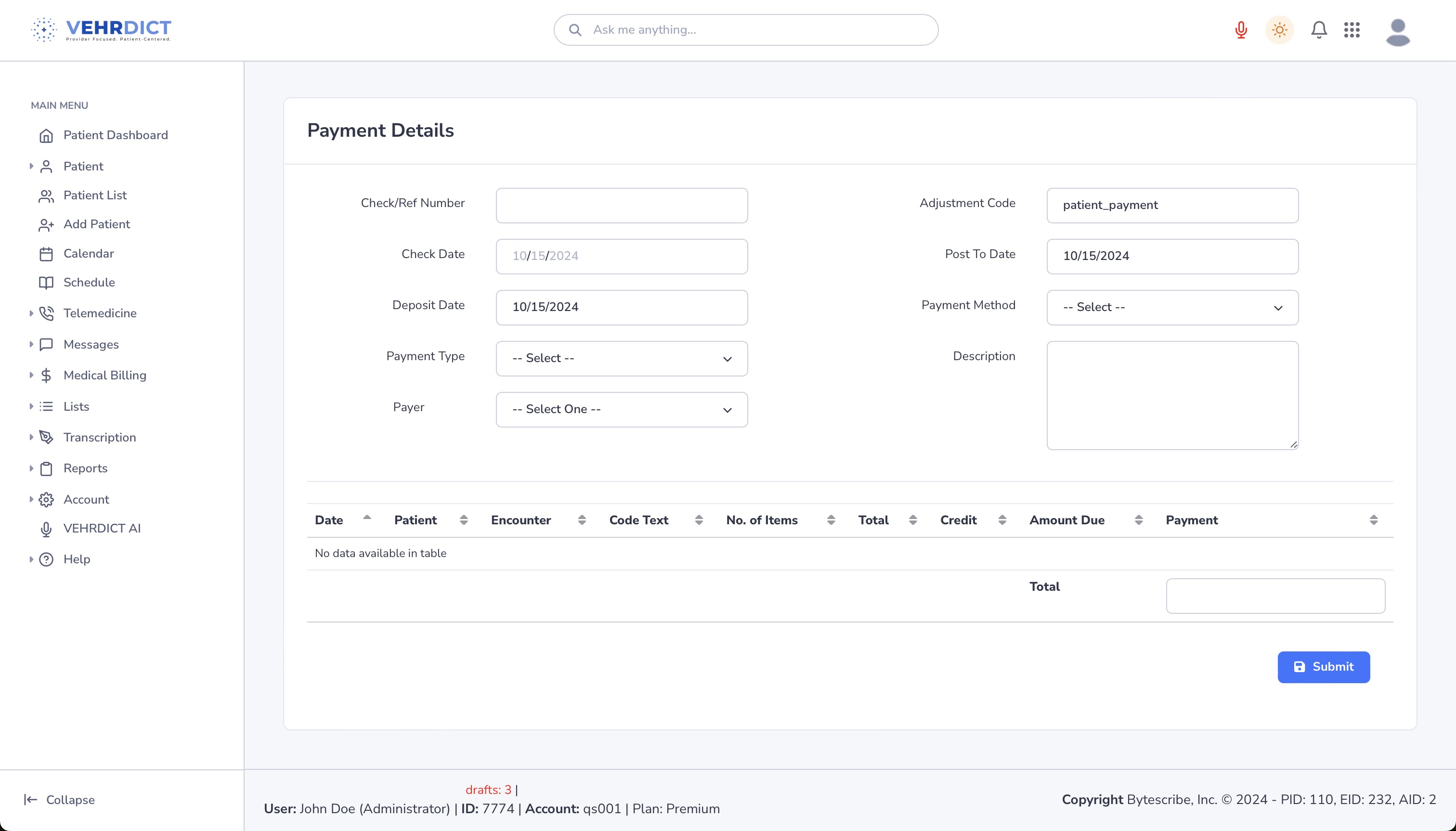
Payment Posting
Once insurance payments are received:
- EOB & ERA Review – Cross-reference with expected charges
- Apply Payments – Match incoming payments with corresponding invoices
Accurate posting ensures financial reporting and patient balance accuracy.
---
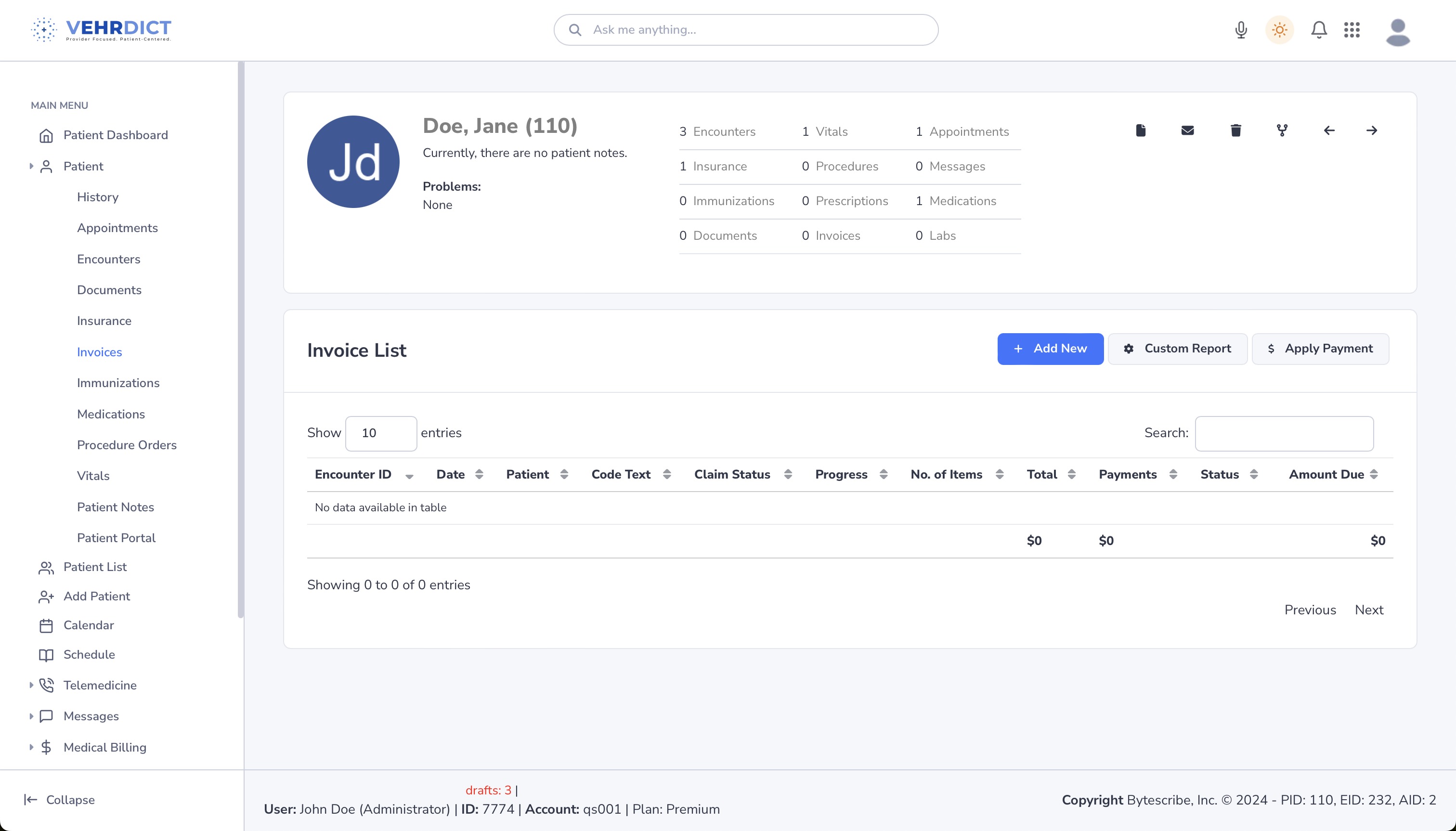
Example Screenshots
Invoice List
Apply Payment
---
Summary
By following these steps in the VEHRDICT system, your practice can streamline billing workflows, minimize errors, and ensure fast and accurate reimbursements for all patient services.